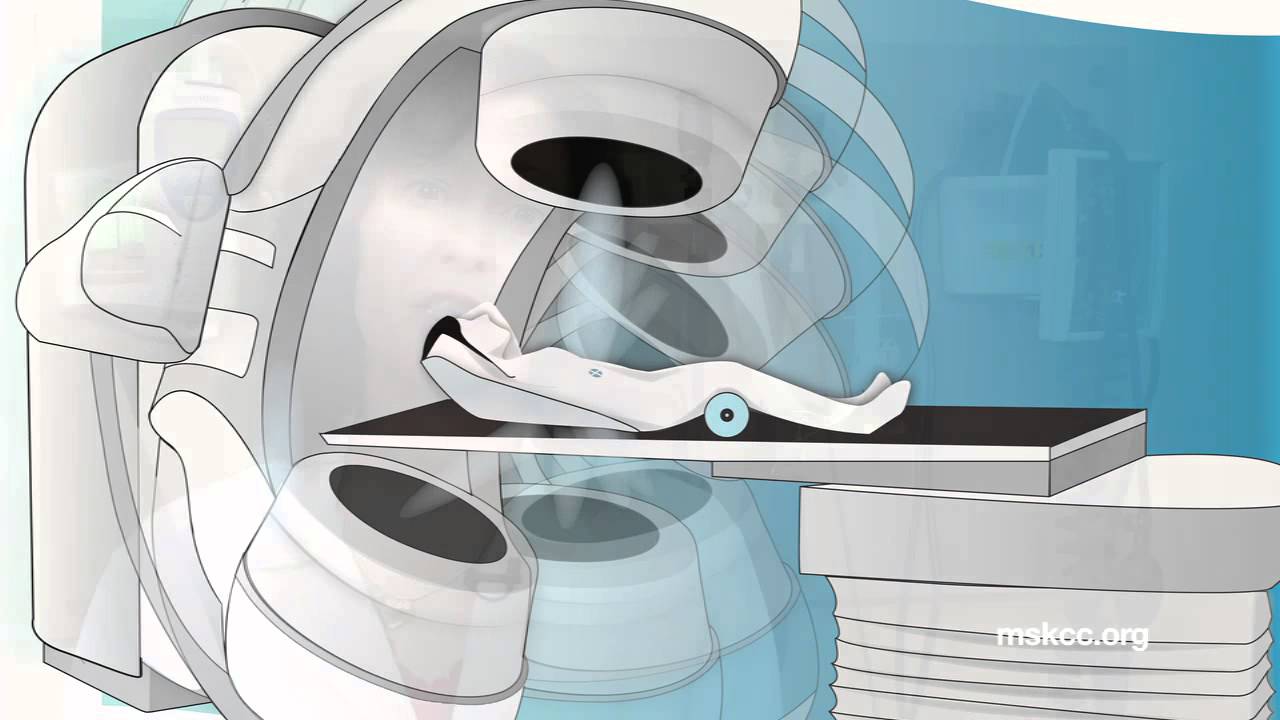
Surgery for Mesothelioma After Radiation Therapy (SMART) has been one of the most talked about upcoming treatments in recent years. The name of the treatment is self-explanatory. The difference between SMART and other radiation plus surgery approaches is its role in making surgery possible for patients with stage 3 and stage 4 mesothelioma.
Late-stage patients receiving this treatment are tripling their survival times in most cases. The first trials of SMART reported a 3-year median survival rate of 84% for stage 3 and 4 patients. That is, the large majority of patients survived 3 years or more. More recent studies have reported median survival times longer than 4 years for patients who received SMART.
This is great news for patients who often receive a prognosis of 1 year or less. It’s especially good for late-stage patients who are often told that surgery is not a possibility. More late-stage patients are now able to benefit from surgery for mesothelioma.
Surgery Still the Best Treatment for Long-term Survival
The best way for any mesothelioma patient to increase their life expectancy is through surgical treatment.
According to Dr. John Cho, “Surgery, despite being the oldest of the three therapeutic modalities, remains the mainstay of curative, ablative therapy.”
There are two surgeries that are similarly effective for Pleural Mesothelioma. The first is the extrapleural pneumonectomy (EPP). In this procedure, a surgeon removes the patient’s affected lung, part of the diaphragm and affected chest lining. It’s the surgery used in the new SMART method.
The second surgical method is the pleurectomy with decortication (P/D). This is the lung-sparing surgical procedure. Surgeons carefully remove mesothelioma tumors from between the lobes of the lung as well as taking out the lining of the lungs.
The P/D and EPP have similar survival benefits. Studies also show that a multimodal surgical approach provides the best chance of survival. Multimodal treatments use more than one type of treatment; for example, a combination of chemotherapy, radiation and surgery. Experts like Dr. Cho agree that surgery plus another form of treatment is best.
A Change In Approach
Now that Mesothelioma Specialists know the benefits of the multimodal approach, the key is to find the right combination of treatments. With SMART, doctors considered an angle that hadn’t been taken yet.
There are limitations to any type of chemotherapy or radiation treatment because of side effects. Doctors must take care in prescribing a certain dose to avoid hurting their patients. The change in philosophy with SMART was the consideration of a very high dose of radiation.
The theory behind SMART was simple: doctors could use higher doses of radiation if they took the irradiated tissue out shortly after. And that’s exactly what they did. Doctors remove the irradiated lung before the radiation can cause damage to other parts of the body.
Why EPP?
The SMART treatment uses the EPP surgery opposed to the P/D. Ever since P/D became as effective as EPP, many doctors switched sides in the treatment debate. Some say there is no place for EPP because it does more harm than good. So why are doctors using EPP in SMART?
The amount of radiation given to the patient before surgery is too high to not remove the lung. If doctors don’t take out the lung in the SMART procedure, the patient would get sick from the radiation.
It’s an aggressive approach. But it’s an approach that is leading to median survival times never seen before in Pleural Mesothelioma patients.
Why Does SMART Work?
SMART works by finding a surgical margin to remove cancerous tumors in the chest. It also prevents something called “spillage” during surgery.
The surgical margin is the necessary amount of tissue that doctors need to remove to get out all the cancer. In skin cancer, for instance, surgeons locate the tumor and cut away extra tissue surrounding the tumor. The idea is that removing the tissue surrounding the tumor will ensure all the cancerous cells surrounding the tumor. After all, there are microscopic cancer cells the surgeon can’t see. Adhering to the surgical margin is a sort of “better safe than sorry” approach.
In mesothelioma surgery, doctors often talk about spillage. Simply put, spillage is when cancer cells are spread by surgery. When a doctor cuts into a tumor, tiny cancer cells “spill” into the nearby tissue. This can lead to the formation of new tumors in distant sites like the other lung.
“We hypothesized that some distant failures were due to incidental tumour spillage during EPP into these areas,” Dr. John Cho said in a study published this June.
These are issues that have hounded mesothelioma surgeons for decades. Mesothelioma isn’t like skin cancer where a surgeon can cut a bigger area around the tumor. Mesothelioma is made up of many small tumors, and it spreads in the chest cavity where a margin isn’t technically possible according to some doctors. Spillage of course is also an issue.
This is where the radiation part of SMART comes in. The heavy dose of radiation creates the margin for surgeons in that all the microscopic cells surrounding the lung are killed off. Surgeons can then remove the lung without cutting into tissue filled with mesothelioma tumors.
Are You Eligible for SMART?
SMART is still in its clinical stages. Experts are still learning who the best candidates for this treatment are, but some factors that could make you a good candidate depends on the histology of your mesothelioma and it’s node involvement.
Most patients accepted for SMART treatment have epithelioid mesothelioma, which is a cell type that spreads slower than other cell types. Patients also usually have no lymph node involvement. Doctors are also learning that the thickness of the patient’s tumors can determine how effective SMART will be. Disease stage seems to be downplayed as an important factor in treatment eligibility.